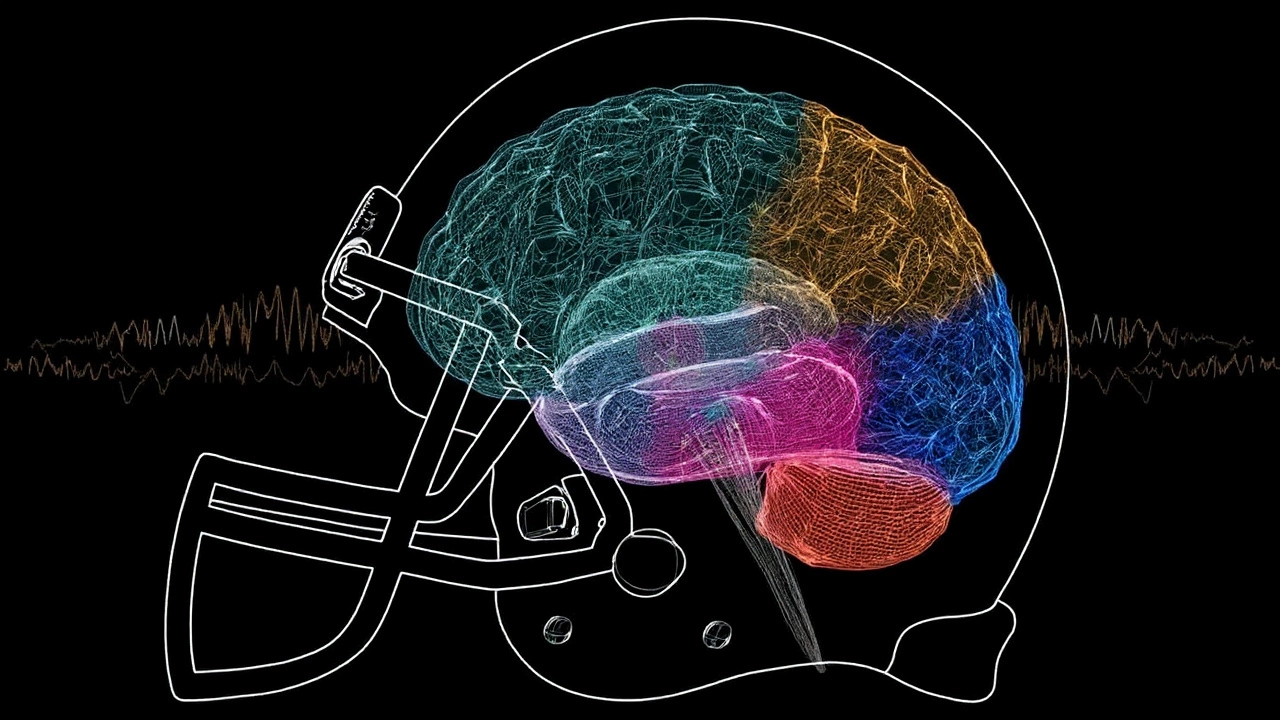
A fringe therapy moves into the sports concussion debate
Pro athletes don’t usually talk about psychedelics when they talk about recovery. Yet behind the scenes, a small but visible group of retired fighters and football players are asking whether ibogaine—a potent psychoactive compound from a West African shrub—can help with the fallout of repeated head trauma. One of the few willing to say it out loud is former UFC flyweight Ian McCall, who has described turning to psychedelic therapy after years of damage in the cage.
Here’s the core tension: concussion and post-concussion syndrome can linger for months or years. Headaches, sleep problems, mood swings, depression, and cognitive fog can outlast a career. Standard care helps many but not all. That’s where ibogaine enters the conversation—not as a cure backed by robust trials, but as a last-resort option some athletes believe eased their symptoms.
Ibogaine is not new. It drew attention in the addiction world decades ago because some patients said it blunted withdrawal and gave them a mental “reset.” Its effect can last 12 to 24 hours and is often described as intense and introspective. For athletes dealing with chronic pain, insomnia, or the emotional blast radius of repeated concussions, that promise of a reset is compelling. It’s also risky, complicated, and not legal in the United States outside of research.
This is where the cross-border reality kicks in. Because ibogaine isn’t FDA-approved, athletes seeking it typically travel to clinics in places like Mexico or Costa Rica. Patient advocates and clinic marketing both point to former pros showing up with a mix of problems—post-concussion symptoms, chronic pain, and, at times, dependence on painkillers. The draw is obvious: conventional options feel tapped out, and the stories—shared on podcasts, in forums, and at conferences—can sound transformative.

What we know, what we don’t, and why the gap matters
Let’s separate hype from facts. Ibogaine’s track record is strongest in addiction, and even there, the research is mostly small studies, observational reports, and case series. It’s intriguing, but it’s not definitive. For brain injuries, the evidence is thinner. There are animal studies and early-stage hypotheses about promoting neuroplasticity and modulating multiple neurotransmitter systems, but there are no large, controlled human trials showing ibogaine reliably treats concussions or chronic traumatic brain injury.
That’s important because the stakes are high. Ibogaine can prolong the heart’s QT interval and trigger arrhythmias, especially in people with underlying cardiac issues or when combined with certain medications. Fatalities have been reported in unregulated settings. Responsible clinics screen patients with EKGs, check electrolytes and liver function, and monitor them throughout the session with medical staff on site. Not all centers meet that bar.
Legal status adds another layer. In the U.S., ibogaine is not approved for medical use. Some countries allow it in clinical or controlled settings; others operate in a gray area. Athletes who go abroad are basically stepping outside the U.S. medical system, which means they’re also stepping outside U.S. patient safeguards and malpractice protections. That doesn’t automatically make it reckless, but it does raise the bar for vetting and oversight.
So why do it? Because for some, the status quo isn’t working. Retired fighters and football players often juggle overlapping issues: pain, sleep disruption, depression, anxiety, and the stress of life after a violent sport. Post-concussion syndrome can magnify all of it. Athletes who have tried ibogaine commonly report, anecdotally, improvements in sleep, mood, and headaches. It’s impossible to know how much of that is the drug, the extended rest, the therapy many pair with it, or the expectancy effect. Without trials, you can’t separate signal from noise.
There’s also a practical mismatch in the science. Most ibogaine research has centered on addiction, not brain injury. The sports world, meanwhile, is moving on several fronts—better concussion protocols, longer return-to-play timelines, and ongoing brain-health studies in retired athletes. Psychedelics are creeping into that conversation, but the sports leagues and regulators are still focused on evidence they can take to a policy committee. Ibogaine isn’t there yet.
Another twist: chemists are developing ibogaine-inspired compounds that may reduce risks. One example is 18-MC (18-methoxycoronaridine), a non-hallucinogenic iboga alkaloid analog that’s been explored for addiction with an eye toward a safer cardiac profile. That’s not a brain-injury therapy today, but it signals where researchers are trying to go—capture potential benefits, strip out the danger.
For athletes considering it anyway, the details matter more than the headlines. If someone is going to seek ibogaine treatment abroad, several nuts-and-bolts questions can change the risk calculation:
- Who does the screening? Ask about EKGs, electrolyte panels, and liver function tests, and whether a physician reviews them.
- What medications are you on? Some antidepressants and other drugs can interact dangerously with ibogaine.
- What happens during dosing? Continuous cardiac and vital sign monitoring should be standard, with a plan for emergencies.
- Who is on site? Look for medical staff with experience in cardiac management and post-anesthesia care.
- What’s the plan after? Integration therapy, sleep hygiene support, and follow-up check-ins make outcomes more stable.
It’s also worth putting ibogaine into a broader playbook. Other avenues under study for post-concussion symptoms include structured cognitive rehab, targeted physical therapy for vestibular and ocular issues, sleep-focused interventions, psychotherapy for mood and anxiety, and, in some cases, medications for headaches and sleep. Psychedelic research is advancing with psilocybin for depression and anxiety, ketamine for treatment-resistant depression and pain, and MDMA-assisted therapy for PTSD—conditions that often overlap with post-concussion syndrome. None of these is a silver bullet, but together they paint a path that’s less about any one compound and more about coordinated care.
There’s a human piece here too. Athletes who open up about psychedelic therapy are usually not chasing a high. They’re chasing normal—seven hours of sleep, headaches that don’t hijack their day, a mood that doesn’t ambush them, a brain that feels like it’s their own again. People latch onto ibogaine because the stories are vivid, because the experience can feel like a break in the clouds. The challenge is turning those stories into data without ignoring the red flags.
Sports will keep having this conversation. The concussion era isn’t going away, and the pressure to find relief isn’t fading. Expect more noise around psychedelics, more clinics advertising, more athletes swapping tips, and—slowly—more studies trying to catch up. Until the science does, ibogaine sits in an uncomfortable place: promising to some, unproven for brain injury, and carrying risks that demand caution, not shortcuts.